Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Excellent outcomes with BCMA directed T cell redirecting therapies in t(11,14) relapsed/ refractory multiple myeloma.
(PA-098) Excellent Outcomes with BCMA Directed T Cell Redirecting Therapies in t(11,14) Relapsed/ Refractory Multiple Myeloma

Asya Varshavsky Yanovsky
Associate Professor
Fox Chase Cancer Center
Introduction:
The t(11,14) translocation is one of the most common primary cytogenetic abnormalities in multiple myeloma, that defines a biologically unique subset of multiple myeloma, characterized by overexpression of cyclin D1 and BCL-2, decreased expression of the adhesion molecule CD56, and increased frequency of light chain disease. While t(11,14) is considered a standard risk cytogenetic abnormality, the data on outcomes of t(11,14) patients is controversial, with evidence of suboptimal response to standard frontline inductions, and improved response with autologous transplant, particularly in Black patients. Outcomes are affected by coexisting cytogenetic abnormalities. Notably, plasma cell leukemia and AL amyloidosis are enriched with t(11,14).
While T cells redirecting therapies (TCRT), including bispecific T cell engagers (BITEs) and CAR-T have revolutionized the outlook for patients with RRMM, little is known about specific effects of these therapies on t(11,14) myeloma.
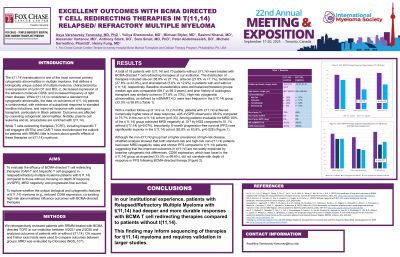
Methods: We retrospectively reviewed patients with RRMM treated with BCMA directed TCRT at our institution between 5/2021 and 2/2025 and analyzed outcomes of patients with or without t(11,14). Chi square and Fisher exact tests were used to compare outcomes between groups. MRD was evaluated by Clonoseq (NGS, 10-6).
Results:
18 pts with t(11,14) and 70 pts without t(11,14) were treated with TCRT (of them ide-cel, 38.9%/27.1%; cilta-cel, 27.8%/17.1%, teclistamab, 27.8%/42.9%, elranatamab 5.6%/12.9% respectively in patients with/without t(11,14)). Median age (68.7 vs 69.3) and prior hx of transplant (77.8% vs 70%) were similar in both groups. High risk cytogenetic abnormalities determined by mSMART4.0 were present in 33.3% patients with t(11,14) vs 58.6% without.
With median follow-up of 14.9/13.2m, numerically more patients achieved at least VGPR in the t(11,14) group (88.9% vs 75.7%, p 0.33). Among MRD evaluable patients, more patients in the t(11,14) group achieved MRD negativity at 10-6 by NGS (80% vs 51.1%, p 0.070). Significantly more patients in the t(11,14) group were progression free at 6 months (93.8% vs 63.8%, p 0.028). While in the non-t(11,14) group more patients had high risk disease, that may confound the results, when non-t(11,14) group was stratified by standard risk and high risk, rates of MRD and 6 months PFS were similar between the two groups and both inferior to the outcomes of the t(11,14) group. While CD56 expression was expectedly lower in the t(11,14) group (33.3% vs 68.6%), CD 56 expression did not correlate with the response to BCMA TCRT.
Conclusions:
In our institutional experience, patients with RRMM with t(11,14) had deeper and more durable responses with BCMA T cell redirecting therapies compared to patients without t(11,14). This finding may inform sequencing of therapies for t(11,14) myeloma and requires validation in larger studies.
