Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Cost per Responder Model of Daratumumab, Bortezomib, Lenalidomide and Dexamethasone (DVRd) for Transplant-Ineligible or Transplant-Deferred Newly Diagnosed Multiple Myeloma
(PA-414) Cost per Responder Model of Daratumumab, Bortezomib, Lenalidomide and Dexamethasone (DVRd) for Transplant-Ineligible or Transplant-Deferred Newly Diagnosed Multiple Myeloma
.jpg)
Santosh Gautam, PhD
Associate Director
Johnson & Johnson
Methods:
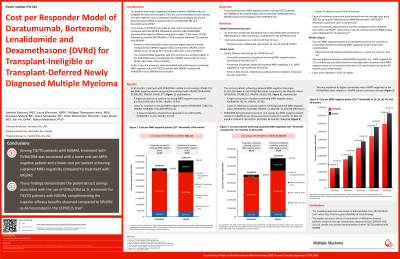
CEPHEUS trial data were used to develop a cost per MRD-negative patient model from a United States (US) mixed payer perspective (80% Medicare, 20% commercial). Model inputs included costs for first-line (1L) and second-line (2L) drug acquisition, medical visits, MRD testing, and adverse event management. Cost per MRD-negative patient was calculated using the cumulative proportion of patients achieving MRD-negative status (10-5 threshold) at 60 months after randomization. Cost per patient achieving sustained MRD negativity (i.e., MRD-negative for ≥12 months) was calculated using the proportion of patients with MRD-negative status on ≥2 occasions that were ≥12 months apart during the 60 months post-randomization. Costs were reported in 2025 US dollars.
Results: At 60 months, the total cost per MRD-negative patient was $640,189 lower for the DVRd/DRd cohort compared to the VRd/Rd cohort. The key drivers for these cost savings were 1) the higher proportion of patients achieving MRD-negative status in DVRd/DRd cohort (60.9%) vs VRd/Rd cohort (39.4%) and 2) the lower 2L treatment costs per MRD-negative patient for the DVRd/DRd cohort ($186,371) compared to the VRd/Rd cohort ($958,840), attributable to the lower proportion of patients having progressed to 2L treatment in the DVRd/DRd (11.2%) vs VRd/Rd cohort (33.3%). The cost per patient achieving sustained MRD-negative status was $1,964,539 lower for the DVRd/DRd cohort relative to the VRd/Rd cohort, primarily attributable to the higher proportion of patients achieving sustained MRD negativity with DVRd/DRd (48.7%) than VRd/Rd (26.3%), and to the lower 2L treatment costs per patient achieving sustained MRD-negative status for the DVRd/DRd cohort ($233,060) compared to the VRd/Rd cohort ($1,436,436).
Conclusions: DVRd/DRd was associated with a lower cost per MRD-negative patient, and cost per patient achieving sustained MRD-negative status compared to VRd/Rd in patients with TIE or TD NDMM. These findings provide evidence of the economic value of 1L DVRd/DRd, complementing the superior efficacy benefits observed compared to VRd/Rd in the CEPHEUS trial.
