Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
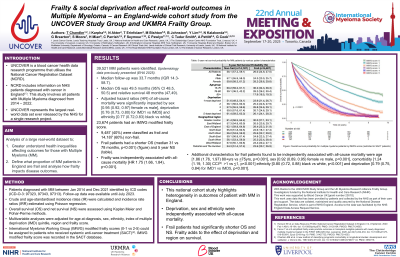
Frailty and social deprivation affect real-world outcomes in Multiple Myeloma (MM) – an England-wide cohort study from the UNCOVER Study Group and UKMRA Frailty Group.
(PA-382) Frailty and Social Deprivation Affect Real-world Outcomes in Multiple Myeloma (MM) – an England-wide Cohort Study from the UNCOVER Study Group and UKMRA Frailty Group

Thea Chandler, MBChB BSc MRCP
Haematology Registrar
Leeds Teaching Hospitals Trust
UNCOVER is a blood cancer health data research programme that utilises the National Cancer Registration Dataset (NCRD). NCRD includes information on all patients diagnosed with all types of cancer in all NHS institutions in England (Int J Epidemiol 2020; 49(1):16– 16h).
Methods:
Data was selected for patients diagnosed with MM (ICD-O-3: 97323, 97343, 97313) between Jan 2014 and Dec 2021 with follow-up until July 2023. Crude and age-standardised incidence rates (IR) were calculated and incidence rate ratios (IRR) estimated using Poisson regression. Overall survival (OS) and net survival (NS) were assessed using Kaplan Meier and Pohar-Perme methods. Multivariable (MV) Cox regression and Fine-Gray models were fitted to estimate all-cause and competing risks mortality. The Poisson model was adjusted for age at diagnosis, gender, ethnicity, index of multiple deprivation (IMD) quintile and region. Cox and Fine-Gray models were additionally adjusted for Charlson co-morbidity index (CCI). International Myeloma Working Group Modified (IMWG) frailty scores (0-1 vs 2- 5) could be assigned to patients who received systemic anti-cancer treatment (SACT). Within this subpopulation, OS and NS was estimated for frail and non-frail groups and a multivariable Cox model fitted that included frailty status.
Results:
39,521 MM patients were identified in total. Crude and age-standardised IR were higher for older people, males and black people. Crude but not age-standardised IR were lower for more deprived areas. Adjusted IRRs increased with age and were lower for females [0.62 (p< 0.001)], less deprived areas [0.95 (p=0.006) for IMD5 vs 1), and all provincial regions vs London [e.g. 0.63 (p< 0.001) for North West]. Median follow-up was 33.7 (IQR: 14.3–58.7) months. 21,987 (55.6%) patients died with median OS 49.5 (48.5–50.5) months and NS
58.7% and 45.3% at 3 and 5 years. Hazard of all-cause mortality was higher for males [1.06 (1.03–1.08)] and increased with age [10.2 (8.1–12.1) for 81–99 compared to < 40], deprivation [1.29 (1.22–1.34) for IMD1 vs 5], comorbidity [1.46 (1.41–1.50) for CCI >1 vs ≤1], and provincial regions vs London [1.21 (1.15–1.28) for North West].
Among the 23,674 (60%) patients with an IMWG frailty score, 9,487 (40%) were classed as frail and 14,187 (60%) non-frail. Frail patients had a shorter OS (median 31 vs 78 months, p< 0.001) and NS (58.1% vs 73.1% at 3 years; 26.0% vs 44.5% at 5 years). This extended to high-risk subgroups defined by deprivation or region (5-year NS: 23.9% vs 51.6% for IMD1; 22.6% vs 55.9% for North East). Frailty was independently associated with all-cause mortality (HR 1.75, p< 0.001).
Conclusions:
Deprivation is associated with a higher probability of MM diagnosis and shorter survival once diagnosed in MV analysis. Living in the capital is associated with a higher probability of MM diagnosis but longer survival once diagnosed. Frailty adds to the effect of deprivation and region and is associated with shorter survival.
