MRD and Biomarkers
Category: MRD and Biomarkers
Minimal Residual Disease Kinetics in Patients with Multiple Myeloma Receiving First Line Treatment and the Association with their Progression-Free Survival; A Retrospective Study of 323 patients
(PA-182) Minimal Residual Disease Kinetics in Patients with Multiple Myeloma Receiving First Line Treatment and the Association with their Progression-Free Survival; A Retrospective Study of 323 patients

Panagiotis Malandrakis, MD, MSc, PhDc (he/him/his)
Clinical and research fellow
Department of Clinical Therapeutics, National and Kapodistrian University of Athens, School of Medicine, Athens, Greece
Minimal residual disease (MRD) has emerged as a highly sensitive tool for evaluating treatment response in multiple myeloma (MM) and is associated with prolonged PFS and OS. Consecutive MRD testing provides critical insight into the depth and durability of response and it drives possible therapeutic decisions.
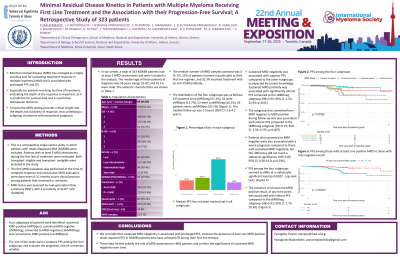
Methods: In this retrospective study we evaluated patients with newly diagnosed MM (NDMM), who were assessed with at least 3 consecutive MRD evaluations in the first line of treatment, irrespective of their transplant status. The first MRD evaluation was performed at the time of complete response and consecutive MRD measurements were done every 6-12 months. Four subgroups of patients were identified: sustained MRD positive (sMRDpos), sustained MRD negative (sMRDneg), converted to MRD negative (conMRDneg) and converted to MRD positive (conMRDpos). The aim of the study was to compare PFS among these groups.
Results:
In our center, a total of 323 NDMM patients had at least 3 MRD assessments and were included in the analysis. The median age of these patients at diagnosis was 59 years (range 35-87) and 55.1% were male. As per risk stratification, our cohort was mostly represented by low-risk patients, and only 16.7% were classified as ISS-3, 7.7% as R-ISS-3 and 4% as R2-ISS-4. The median number of MRD samples assessed was 5 (3-13). 25% of patients received a quadruplet as their first line regimen, and 32.3% received treatment with an anti-CD38 antibody. The distribution of the four subgroups was as follows: 165 patients were sMRDneg (51.1%), 41 were sMRDpos (12.7%), 52 were conMRDneg (16.1%), 65 patients were conMRDpos (20.1%). The median follow-up was 3.9 years (95% CI: 3.6-4.2 years). Median PFS has not been reached yet in all studied subgroups. Sustained MRD negativity was associated with superior PFS compared to the other subgroups, as expected by current knowledge. Sustained MRD positivity was associated with significantly inferior PFS compared to the sMRDneg subgroup (HR=5.92; 95% CI: 1.53-22.94; p=0.01). The subgroup that converted from MRD negative to MRD positive during follow-up was also associated with inferior PFS compared to the sMRDneg subgroup (HR=5.19; 95% CI: 1.58-17.05, p=0.007). Patients who converted to MRD negative were also associated with a worse prognosis compared to those with sustained MRD negativity, but this difference did not reach a statistical significance to-date (HR=2.85; 95% CI: 0.58-14.0; p=0.196]. The presence of at least one MRD positive result, at any time-point, was associated with inferior PFS compared to the sMRDneg subgroup (HR=5.93; 95% CI: 1.73-20.30; p=0.0046).
Conclusions:
We conclude that sustained MRD negativity is associated with prolonged PFS, whereas the presence of even one MRD positive result impaired PFS in NDMM patients who have achieved CR during their first line therapy. These data further solidify the role of MRD assessment in MM patients and confirm the significance of sustained MRD negativity over time.
