Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
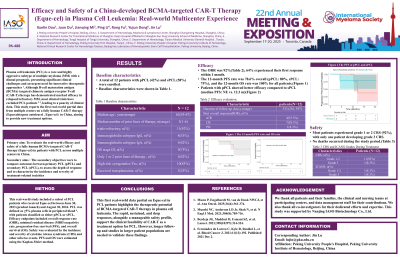
Efficacy and Safety of a China-developed BCMA-targeted CAR-T Therapy (Eque-cel) in Plasma Cell Leukemia: Real-world Multicenter Experience
(PA-488) Efficacy and Safety of a China-developed BCMA-targeted CAR-T Therapy (Eque-cel) in Plasma Cell Leukemia: Real-world Multicenter Experience

Jin Lu, MD
Professor
Peking University People’s Hospital, Peking University Institute of Hematology, National Clinical Research Center for Hematologic Disease,Beijing,China; Department of Hematology, Fu Xing Hospital, Capital Medical University, Beijing, China.
Plasma cell leukemia (PCL) is a rare and highly aggressive subtype of multiple myeloma (MM) with a dismal prognosis, presenting significant clinical challenges and an urgent need for innovative therapeutic approaches. Although B-cell maturation antigen (BCMA)-targeted chimeric antigen receptor T-cell (CAR-T) therapy has demonstrated marked efficacy in relapsed/refractory MM, most clinical trials have excluded PCL patients, leading to a paucity of clinical data. This study reports the first real-world partial data from multiple centers on a fully human CAR-T therapy (Equecabtagene autoleucel,Eque-cel) in China, aiming to provide new treatment options.
Methods:
This real-world study included a subset of PCL patients who received Eque-cel between June 30, 2023 (product launch) and August 30, 2024. PCL was defined as ≥5% plasma cells in peripheral blood, with patients classified as either primary (pPCL) or secondary PCL (sPCL). Efficacy endpoints included overall response rate (ORR), minimal residual disease (MRD) negativity rate, progression-free survival (PFS), and overall survival (OS). Safety was evaluated by the incidence and severity of cytokine release syndrome (CRS) and other adverse events. PFS and OS were estimated using the Kaplan-Meier method.
Results:
A total of 12 patients with pPCL (42%) or sPCL (58%) were enrolled. The median age was 62 years (range: 55–67), and the median number of prior lines of therapy was 3 (range: 1–6), with 92% being triple-refractory. Immunoglobulin subtypes: 33%IgG (4/12), 42% IgA (5/12). Advanced disease was frequent: 75% (9/12) were DS stage III. 42% (5/12) had received only 1 or 2 prior lines of therapy. High-risk cytogenetic features were observed in 83% (10/12). Three patients had undergone prior transplantation.
With a median follow-up of 333 days (range: 281–397), the ORR was 92%, with 92% of patients achieving complete response or better (CR/sCR). 64% experienced their first response within 1 month, with a median duration of response of 282 days (range: 236–339). At the last follow-up, the median PFS and OS had not been reached. Notably, patients with pPCL showed better efficacy compared to sPCL (median PFS: NE vs. 12.3 m). The 12-month PFS was 78.6% overall (pPCL: 80%, sPCL: 75%), and the 12-month OS was 100% for all patients.
Regarding safety, most patients experienced grade 1 or 2 CRS (92%), with only one patient developing grade 3 CRS. ICANS occurred in 2 patients, including one grade 3 event. Most patients achieved hematologic recovery within 90 days post-infusion. No deaths occurred during the study period.
Conclusions:
This first real-world data partial on Eque-cel in PCL patients highlights the therapeutic potential of BCMA-targeted CAR-T therapy in plasma cell leukemia. The rapid, sustained, and deep responses, alongside a manageable safety profile, support the clinical feasibility of CAR-T as a treatment option for PCL. However, longer follow-up and studies in larger patient populations are needed to validate these findings.
