Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Time Toxicity associated with Selinexor-Pomalidomide-Dexamethasone versus Other Treatments for Relapsed/Refractory Multiple Myeloma
(PA-496) Time Toxicity Associated with Selinexor-pomalidomide-dexamethasone versus Other Treatments for Relapsed/refractory Multiple Myeloma

David Ray, PharmD, MBA, MPH
Executive Director, Global HEOR
Karyopharm Therapeutics
Introduction:
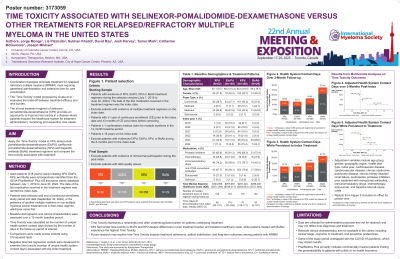
Combination therapies, many of which require injectable administration and extensive time for care coordination, dominate treatment for relapsed/refractory multiple myeloma (RRMM). The ‘Time Toxicity’ model proposed by Gupta et al. evaluated the trade-off between treatment efficacy and time burden. We applied this framework of ‘Time Toxicity’ to patients with RRMM treated with selinexor-pomalidomide-dexamethasone (XPd) versus other common treatments.
Methods:
This retrospective, observational cohort study compared patients initiating XPd, elotuzumab-pomalidomide-dexamethasone (EloPd), carfilzomib-pomalidomide-dexamethasone (KPd) or a bispecific antibody (BsAb; teclistamab, talquetamab, elranatamab) treatment for RRMM within the IQVIA Pharmetrics® Plus US insurance claims database between July 2019 and June 2024 (first treatment= “index date”). Patients were required to have ≥1 year of continuous enrollment (CE) prior to and ≥3 months of CE post-index. Time Toxicity was based on health system contact days, calculated as the total number of unique days in contact with the health system divided by the length of the variable post-index period and summarized by care setting (e.g., inpatient, outpatient, etc.). A hierarchy was applied to avoid double counting days for patients with multiple care settings on the same day. Percent of unique health system contact days post-index was used to compare the Time Toxicity associated with the different treatment options. Analysis of variance (ANOVA) test (mean), non-parametric Kruskal-Wallis Test (median), and chi-square tests (proportions) were used to determine significant differences across cohorts.
Results:
The sample included 62, 155, 356 and 26 patients treated with XPd, EloPd, KPd, and BsAb, respectively. Mean age ranged from 65.4 years for KPd to 69.2 years for EloPD with 52-58% female. Proportion with commercial payers ranged from 28% for EloPD to 45% for KPd while proportion with Medicare Advantage ranged from 42% for KPd to 62% for EloPD. Median baseline all-cause cost for the year prior to starting treatment as an indicator of future utilization was highest for the XPd group ($333,959) followed by BsAb ($289,300), KPd ($281,424) and EloPd ($257,952) (p=0.014). Median follow-up time in days ranged from 149 days for BsAb to 435 days for EloPD. Mean Time Toxicity was significantly different across treatments with the highest percentage of unique health system contact days observed for BsAb (20.6%), followed by KPd (14.6%), EloPd (12.9%) and XPd (12.5%) (p < 0.001). The differences were driven by inpatient contact days among patients treated with BsAb (13.6%) whereas all other treatments had rates below 9% (p < 0.001).
Conclusions: Results suggest the all-oral treatment option of XPd could be beneficial when considering Time Toxicity associated with treatments for patients with RRMM. The EMN29 trial (NCT05028348) investigating XPd vs EloPd among patients with RRMM will provide further insight into treatment efficacy.
