Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
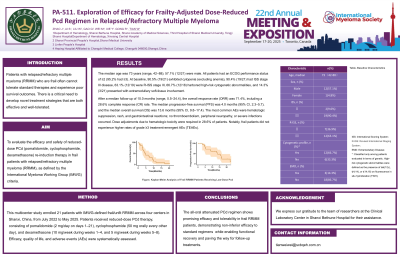
Exploration of Efficacy for Frailty-Adjusted Dose-Reduced Pcd Regimen in Relapsed/Refractory Multiple Myeloma
(PA-511) Exploration of Efficacy for Frailty-adjusted Dose-reduced Pcd Regimen in Relapsed/refractory Multiple Myeloma
Weiwei Tian, Chief Physician, MD, PhD Supervisor at Shanxi Medical University
Chief Physician、Chief of Hematology Department
Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences,Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University
Methods:
This multicenter study enrolled 21 patients with IMWG-defined frail/unfit RRMM across four centers in Shanxi, China, from July 2022 to May 2025. Patients received reduced-dose PCd therapy, consisting of pomalidomide (2 mg/day on days 1–21), cyclophosphamide (50 mg orally every other day), and dexamethasone (10 mg/week during weeks 1–4, and 5 mg/week during weeks 5–8). Efficacy, quality of life, and adverse events (AEs) were systematically assessed.
Results:
The median age was 73 years (range, 42–88); 57.1% (12/21) were male. All patients had an ECOG performance status of ≥2 (95.2% had ≥3). At baseline, 90.5% (19/21) exhibited cytopenia (excluding anemia), 90.4% (19/21) had ISS stage III disease, 63.1% (12/19) were R-ISS stage III, 66.7% (12/18) harbored high-risk cytogenetic abnormalities, and 14.3% (3/21) presented with extramedullary soft-tissue involvement.After a median follow-up of 10.0 months (range, 0.5–24.4), the overall response rate (ORR) was 71.4%, including a 28.6% complete response (CR) rate. The median progression-free survival (PFS) was 4.0 months (95% CI, 2.3–5.7), and the median overall survival (OS) was 13.6 months (95% CI, 9.8–17.4). The most common AEs were hematologic suppression, rash, and gastrointestinal reactions; no thromboembolism, peripheral neuropathy, or severe infections occurred. Dose adjustments due to hematologic toxicity were required in 28.6% of patients. Notably, frail patients did not experience higher rates of grade ≥3 treatment-emergent AEs (TEAEs).
Conclusions: The all-oral attenuated Pcd regimen demonstrates promising efficacy and tolerability in frail RRMM patients, showing non-inferior efficacy compared to standard regimens while providing a therapeutic platform for treatment-failed patients to improve their clinical status
