Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
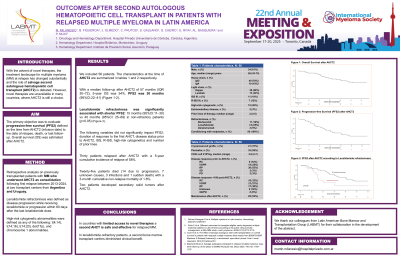
OUTCOMES AFTER SECOND AUTOLOGOUS HEMATOPOIETIC CELL TRANSPLANT IN PATIENTS WITH RELAPSED MULTIPLE MYELOMA IN LATIN AMERICA
(PA-495) Outcomes After Second Autologous Hematopoietic Cell Transplant in Patients with Relapsed Multiple Myeloma in Latin America

Martín Milanesio
Hematologist
Hospital Privado Universitario de Córdoba, Argentina
Introduction:
With the advent of novel therapies, the treatment landscape for multiple myeloma (MM) at relapse has changed substantially and the role of salvage second autologous hematopoietic cell transplant (AHCT2) is debated. However, novel therapies are unavailable in many countries, where AHCT2 is still a choice. We conducted a retrospective analysis of MM patients who underwent AHCT2 after first relapse at two Latin American transplant centers.
Methods:
Retrospective analysis on previously transplanted patients with MM who underwent AHCT2 as consolidation following first relapse between 2013-2024, at two transplant centers from Argentina and Uruguay. The primary objective was to evaluate progression-free survival (PFS2) defined as the time from AHCT2 (infusion date) to the date of relapse, death, or last follow-up. Also, PFS after first transplant (PFS1) was calculated.Overall survival (OS) was estimated after AHCT2.
Results:
Fifty-six patients were included: 70% IgG, 69% kappa light chain, 19% ISS III, 12% R-ISS III and 26% high-risk cytogenetic at diagnosis. The median PFS1 was 51 months. At the time of AHCT2 the median age was 59 years (range 43–73) and the median of prior lines of therapy was 2 (range 2–5). Prior exposure to bortezomib, thalidomide, lenalidomide and daratumumab was 54 (96%), 47 (84%), 32 (57%), and 8 (14%), respectively, while 19%, 19%, 25%, and 5% were refractory to these drugs, respectively. Three patients were triple refractory. All patients received conditioning with melphalan single-drug and cryopreserved grafts in 21 cases (37%). Disease response prior to AHCT2 was: complete response (CR) 8 (14%), very good partial response (VGPR) 14 (25%), partial response (PR) 30 (53%), stable disease (SD) 2 (3%) and progressive disease (PD) 2 (3%). At day +100 post AHCT2 response rates were: CR 18 (32%), VGPR 12 (21%), PR 17 (30%), and no cases of PD (unknown in 9 cases). Maintenance therapy after AHCT2 was administered in 29 (52%) (lenalidomide monotherapy 20/29). With a median follow-up after AHCT2 of 57 months (IQR 30–72), 5-year OS was 54%. PFS2 was 30 months (95%CI:22–41). Lenalidomide refractoriness was significantly associated with shorter PFS2: 15 months (95%CI:11–30) vs 40 months (95%CI:25–69) in non-refractory patients (p< 0.05). Median PFS2 in patients who received maintenance after AHCT2 was 30 months vs 15 months in those who did not (p=0.3). The following variables did not significantly impact PFS2: duration of response to the first AHCT, disease status prior to AHCT2, ISS, R-ISS, high-risk cytogenetics and number of prior lines. Thirty patients relapsed after AHCT2 with a 5-year cumulative incidence of relapse of 58%. Twenty-five patients died (14 due to progression, 7 unknown causes, 3 infections and 1 sudden death) with a 3-month cumulative non-relapse mortality of 1.8%. Two patients developed secondary solid tumors after AHCT2.
Conclusions:
In countries with limited access to novel therapies a second AHCT is safe and effective for relapsed MM.
