Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
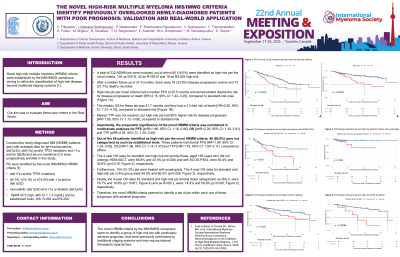
The novel high-risk multiple myeloma IMS/IMWG criteria identify previously overlooked newly-diagnosed patients with poor prognosis: validation and real-world application
(PA-391) The Novel High-risk Multiple Myeloma IMS/IMWG Criteria Identify Previously Overlooked Newly-diagnosed Patients with Poor Prognosis: Validation and Real-world Application

Ioannis Ntanasis-Stathopoulos, MD (he/him/his)
Clinical and research fellow
Department of Clinical Therapeutics, National and Kapodistrian University of Athens, School of Medicine, Athens, Greece
Νovel high-risk multiple myeloma (HRMM) criteria were established by the IMS/IMWG consensus, aiming to refine the classification of high-risk disease beyond traditional staging systems. Our aim was to evaluate these new criteria in the Real World.
Consecutive newly-diagnosed MM (NDMM) patients (pts) with available data for IgH translocations, del(1p32), del(17p) and/or TP53 mutations and +1q, and for Sβ2M and serum creatinine (Cr) were prospectively enrolled in this study. Pts were stratified by the novel IMS/IMWG HRMM criteria [del(17p) and/or TP53 mutations - t(4;14), t(14;16) or t(14;20) with +1q and/or del(1p32) - or monoallelic del(1p32) and +1q or biallelic del(1p32) - or Sβ2M ≥5.5 mg/L with Cr < 1.2 mg/dL] and by established tools: ISS, R-ISS and R2-ISS. A total of 332 NDMM pts were included, out of which 60 (18.0%) were identified as high-risk per the novel criteria, 103 as ISS III, 42 as R-ISS III and 18 as R2-ISS high-risk. After a median follow-up of 37.5 months, there were 79 (23.8%) disease progression events and 72 (21.7%) deaths recorded. High-risk pts per novel criteria had a median PFS of 25.5 months and demonstrated double the risk for disease progression or death [HR=2.15, 95% CI: 1.42–3.25], compared to standard-risk ones. The median OS for these pts was 30.0 months and they had a 2.5-fold risk of death [HR=2.50, 95% CI: 1.51–4.15], compared to standard-risk. Median TTP was not reached, but high-risk pts had 85% higher risk for disease progression [HR=1.85, 95% CI: 1.12–3.08], compared to standard-risk. Importantly, the prognostic significance of the novel HRMM criteria was maintained in multivariate analyses for PFS [aHR=1.86, 95% CI: 1.18–2.96], OS [aHR=2.26, 95% CI: 1.30–3.91] and TTP [aHR=2.04, 95% CI: 1.20–3.46]. Out of the 60 patients identified as high-risk per the novel HRMM criteria, the 48 (80.0%) were not categorized as such by established tools. These patients had dismal PFS [HR=1.94, 95% CI: 1.24–3.05], OS [HR=1.99, 95% CI: 1.14–3.47] and TTP [HR=1.79, 95% CI: 1.04–3.11], compared to others. The 4-year OS rates for standard and high-risk pts among those: aged >65 years who did not undergo HDM-ASCT, were 66.8% and 43.3% (p=0.020) and with ECOG PS≥2, were 60.4% and 30.9% (p=0.020), respectively. Furthermore, 104 (31.3%) pts were treated with quadruplets. The 4-year OS rates for standard and high-risk pts in this group were 94.9% and 66.5% (p=0.030), respectively. Finally, the 4-year OS rates for standard and high-risk pts among those categorized: as ISS-2, were 79.7% and 19.8% (p < 0.001) and as R-ISS 2, were: 74.9% and 56.9% (p=0.030), respectively. Therefore, the novel HRMM criteria seemed to identify a set of pts within each one of these subgroups with adverse prognosis. The novel HRMM criteria by the IMS/IMWG consensus seem to identify a group of high-risk pts with particularly adverse prognosis, that were previously overlooked by traditional staging systems and may require tailored therapeutic approaches.
Methods:
Results:
Conclusions:
