Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
PRO-Guided Treatment Readiness for Daratumumab in Myeloma: Feasibility and Accuracy
(PA-152) PRO-Guided Treatment Readiness for Daratumumab in Myeloma: Feasibility and Accuracy

Thomas Lund, PhD
Head of Department
Department of Medicine, Hematological Section, Vejle Hospital, Denmark
For patients with multiple myeloma receiving daratumumab, standard pre-treatment evaluations typically rely on in-person clinical assessments. However, as outpatient cancer care increasingly explores digital and patient-centered solutions, the use of Patient Reported Outcome (PRO) data to assess treatment readiness has gained interest. This study aimed to investigate whether PRO data can reliably replace routine clinical evaluations prior to daratumumab administration, and to assess the overall feasibility of implementing such a strategy in daily practice.
Methods:
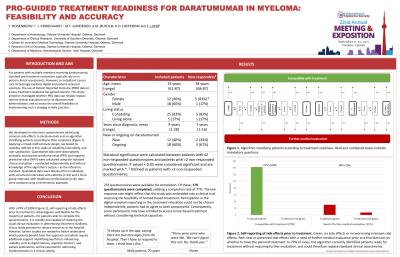
We developed an electronic questionnaire addressing common side effects to daratumumab and an algorithm stratifying patients according to their responses. Applying a mixed-method study design, we tested its usability, defined in this study as reliability, learnability, and user satisfaction. Quantitative data were descriptively analyzed, and positive predictive value and negative predictive value were calculated using the standard clinical evaluation – conducted independently and without knowledge of the algorithm’s output – as the reference standard. Qualitative data were obtained from individual, semi-structured interviews with patients (n=19) and a focus group interview with healthcare professionals (n=4); data were analyzed using a hermeneutic approach.
Results: With a positive predictive value of 100%, we found the questionnaire able to identify patients physically fit for treatment without need for further consultation. Of 179 completed questionnaires, the algorithm recommended treatment in 142 cases, thus demonstrating the potential of PRO data to replace standard clinical evaluations in 79% of cases. However, with a patient response rate of 77%, we also found that some patients were unable to report side effects digitally using a smartphone themselves. With respect to gender and age we found no statistical difference between patients being able or unable to complete the questionnaires. Qualitative findings were confirmative suggesting that patients had very different perceptions of registering their side effects themselves.
Conclusions:
Self-reporting of side effects prior to treatment is advantageous and flexible for the majority of patients. For patients able to complete the questionnaires, it is reliable and capable of replacing the usual clinical evaluation in determining treatment readiness. It thus holds potential to release resources at the hospital. However, further studies are needed to better understand which patients benefit from this approach and which require additional support. Identifying key factors influencing usability, such as digital literacy, cognitive function, and patient preferences, will be essential for optimizing implementation in a clinical setting.
