Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
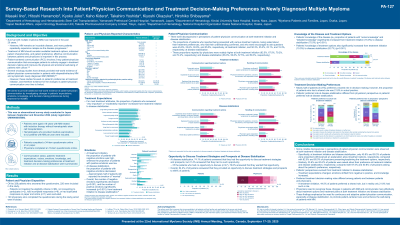
Survey-based research into patient-physician communication and treatment decision-making preferences in newly diagnosed multiple myeloma
(PA-127) Survey-based Research into Patient-physician Communication and Treatment Decision-making Preferences in Newly Diagnosed Multiple Myeloma
.jpg)
Masaki Iino (he/him/his)
Director at Dpt. Hematology and Hematopoietic Stem Cell Transplantation
Yamanashi Prefectural Central Hospital
Introduction:
We aimed to clarify the realities of patient-physician communication and investigate changes in patients’ expectations, emotions, knowledge, and decision-making preferences during treatment for newly diagnosed multiple myeloma (NDMM).
Methods: An observational survey was conducted between September and November 2024 in Japan. Patients with NDMM who had not received hematopoietic stem cell transplantation completed a 34-item survey covering communication status, treatment expectations, values, emotions, disease knowledge, and decision-making preferences. Hematologists completed an 18-item survey on their perspectives about communication and treatment decisions. Responses were analyzed in two phases: at start of treatment and at disease stabilization.
Results:
A total of 220 patients (median age: 73.5 years) and 120 hematologists were included. Most patients had been diagnosed with multiple myeloma for ≥3 years. Common induction regimens reported by patients were Bd (bortezomib, dexamethasone) (19.1%), DLd (daratumumab, lenalidomide, dexamethasone) (11.8%), and Ld (lenalidomide, dexamethasone) (11.4%). Both at the start of treatment and at disease stabilization, the proportion of patients being presented or receiving explanations about treatment options was 45.9% and 50.3%, respectively, and those asked about their preference was 23.6% and 25.2%, respectively. Conversely, these proportions were notably higher for physicians at the start of treatment and at disease stabilization: 82.5% and 65.0% presented or explained about treatment options, and 67.5% and 50.8% asked for patients’ preferences, respectively. Overall, the number of negative emotions (e.g. “worried” and “confused”) significantly decreased at disease stabilization (p< 0.001), whereas the number of positive emotions (e.g. “optimistic/hopeful,” “confident,” and “excited)”, which were initially low, significantly increased (p< 0.001). Patients’ knowledge about the disease and treatment options significantly increased from the start of treatment to disease stabilization (p< 0.001), with “some” or “detailed knowledge” rising from 15.0% to 75.0% for the disease and from 15.0% to 62.7% for treatment options. Patients’ expectations for most treatment attributes, such as “improved quality of life,” “longer survival,” and “long time to recurrence,” increased from the start of treatment to disease stabilization. Nearly half of patients (44.5%) preferred a shared role in decision-making; however, in actual practice, the proportion of patients who had a shared role was 21.8%.
Conclusions:
A disparity was observed in perceptions of communication between patients and physicians, and patients’ expectations, emotions, and knowledge changed from the start of treatment to disease stabilization. Physicians should recognize these changes in patients and communicate more effectively about treatment options and plans at each treatment phase, including when the disease is stabilized.
