Nursing and Allied Health Symposium
Category: Nursing & Allied Health Symposium
Energy and Macronutrient Deficits in Multiple Myeloma: The Hidden Burden Across the Disease Spectrum
(NSP-07) Energy and Macronutrient Deficits in Multiple Myeloma: The Hidden Burden Across the Disease Spectrum

Nancy Sahni, PhD Nutrition, HOD Dept. of Dietetics, PGIMER, Chandigarh, 25 years of experience
Chief Dietician
PGIMER , Chandigarh
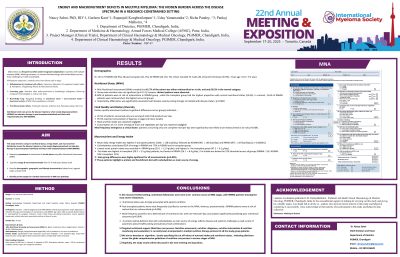
Methods: This cross-sectional observational study was conducted over one month at a tertiary care teaching hospital in North India, a representative setting. All patients diagnosed with MM (IMWG criteria) and treated were included. Nutritional status was assessed with the Mini Nutritional Assessment (MNA). Dietary intake was assessed using a 3-day recall and analyzed for energy and macronutrients. Patients were grouped into newly diagnosed on induction therapy, post-transplant on maintenance, and RRMM. Statistical analysis included Chi-square and ANOVA tests.
Results:
Seventy-five patients were evaluated (median age 61 years, male-to-female ratio 8:7): 42 on induction, 20 post-transplant, and 13 RRMM. Malnutrition was most prevalent in RRMM (50%), while 71.4% of newly diagnosed patients were at risk. Post-transplant patients had the most favorable nutritional profile, with 45.7% well-nourished (Chi-square = 21.04, p = 0.0003).
Mean daily energy intake was highest in transplant patients (1250 kcal), followed by MM (986 kcal) and RRMM (780 kcal) (ANOVA F = 128.8, p < 0.000001). Macronutrient intake varied significantly (Protein: p < 0.00001; Carbohydrates: p = 0.00012; Fat: p < 0.00001).
Compared to the estimated TEE of 1574 kcal and protein requirement of 78 g/day, RRMM patients had the greatest deficits—50.4% in energy and 82.4% in protein. MM patients had 37.4% and 62.2% deficits, respectively, while transplant patients had 20.6% and 43.8% deficits.
Carbohydrates contributed 82% of energy in RRMM, 70% in MM, and 65% in transplant—above the ideal (~60%). Fat intake was below the 22% threshold across all groups (RRMM: 11%, MM: 18%, transplant: 21%). These patterns highlight a carbohydrate-heavy, protein- and fat-deficient intake, notably in RRMM.
Conclusions: In this resource-limited setting, nutritional deficiencies are common across all MM stages, with RRMM patients showing the most severe imbalances. Even post-transplant patients had notable deficits. The dominance of high-carbohydrate, low-protein, low-fat diets reflects disease and systemic challenges. Targeted nutritional support is essential in routine myeloma care.
