Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
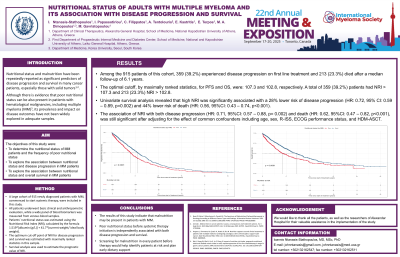
Nutritional status of adults with multiple myeloma and its association with disease progression and survival
(PA-147) Nutritional Status of Adults with Multiple Myeloma and Its Association with Disease Progression and Survival

Ioannis Ntanasis-Stathopoulos, MD (he/him/his)
Clinical and research fellow
Department of Clinical Therapeutics, National and Kapodistrian University of Athens, School of Medicine, Athens, Greece
Nutritional status and malnutrition have been repeatedly reported as significant predictors of disease progression and survival in many cancer patients, especially those with solid tumors. Although there is evidence that poor nutritional status can be also present in patients with hematological malignancies, including multiple myeloma (MM), its prevalence and impact on disease outcomes have not been widely explored in adequate samples.
Methods:
A large cohort of 915 newly diagnosed patients with MM, commenced to start systemic therapy, were included in this study. All patients underwent basic clinical and anthropometric evaluation, while a wide panel of blood biomarkers was measured from venous blood samples. Patients’ nutritional status was estimated using the Nutritional Risk Index (NRI), calculated by the formula 1.519*[albumin (g/L)] + 41.7*(current weight/ ideal body weight). The optimum cut-off point of NRI for disease progression and survival was estimated with maximally ranked statistics in this sample. Survival analysis was then used to estimate the prognostic value of NRI.
Results:
Among the 915 patients of this cohort, 359 (39.2%) experienced disease progression on first line treatment and 213 (23.3%) died after a median follow-up of 6.1 years. The optimal cutoff, by maximally ranked statistics, for PFS and OS, were: 107.3 and 102.8, respectively. A total of 359 (39.2%) patients had NRI > 107.3 and 213 (23.3%) NRI > 102.8. Univariate survival analysis revealed that high NRI was significantly associated with a 28% lower risk of disease progression (HR: 0.72, 95% CI: 0.59 – 0.89, p=0.002) and 44% lower risk of death (HR: 0.56, 95%CI: 0.43 – 0.74, p< 0.001). The association of NRI with both disease progression (HR: 0.71, 95%CI: 0.57 – 0.88, p= 0.002) and death (HR: 0.62, 95%CI: 0.47 – 0.82, p< 0.001), was still significant after adjusting for the effect of common confounders including age, sex, R-ISS, ECOG performance status, and HDM-ASCT.
Conclusions:
The results of this study indicate that malnutrition may be present in patients with MM, and that poor nutritional status before systemic therapy initiation is independently associated with both disease progression and survival. Screening for malnutrition in every patient before therapy would help identify patients at risk and plan early dietary support in parallel to their anti-myeloma treatment.
