Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
Current survival and causes of mortality of myeloma patients in real word setting
(PA-132) Current Survival and Causes of Mortality of Myeloma Patients in Real Word Setting

Leah Kogan, BSc (she/her/hers)
Medical Student
University of Limerick
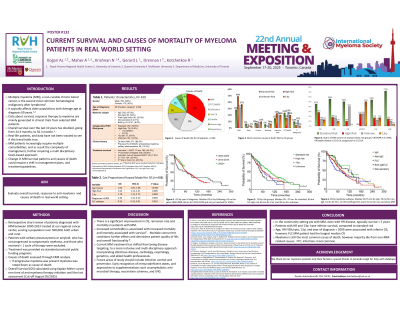
Introduction: Therapy of multiple myeloma (MM) is constantly improving, and the overall survival (OS) rate is now over 5 years with many patients (pts) living 10 years or more. The rate of comorbidities at time of MM diagnosis is estimated to be 54%; with longer survival rates this finding impacts the long-term clinical management of these pts. In our study we aimed to evaluate the OS of MM pts and identify causes of death in a real-world setting.
Methods:
This retrospective chart review included patients diagnosed with MM between 2000-2023 treated at our regional cancer center, serving a population over 500,000, both urban and rural. Pts with solitary plasmacytoma or amyloid, who has not progressed to symptomatic myeloma, and those who received < 1 cycle of therapy were excluded. Treatment was provided via standard provincial public funding programs. Causes of death were assessed by electronic medical records. If a pt had progressive myeloma at the time of death, the cause of death was considered related to myeloma, irrespective of reported cause. OS was calculated by Kaplan-Meier curves from time of anti-myeloma therapy initiation until the last assessment (cut off May 05, 2025) or death.
Results:
429 pts were evaluated. Median age was 68 [range 41 to 96] years, male/female ratio 1.4: 1. 13.5% of MGUS/smoldering myeloma or isolated plasmacytoma pts progressed to symptomatic myeloma. IgG myeloma was the most common subtype (47.3%), followed by non-IgG (20%) and free light chain (20.9%) isotypes. 68.54% of pts had standard-risk FISH/cytogenetics while 18.4% had known high-risk (del17p and/or t[4;14]) features. 254 patients died. While MM was most common cause of death (33.6%), most pts died from non-MM related causes, including failure to thrive (22.05%), infections (17.71%) , secondary malignancies (8.66%), cardiac issues (7.48%), bleeding (5.12%), and non-infectious respiratory causes (4.33%). Disease status at the last assessment included: CR/VGPR in 57.58%, PR/stable disease in 19.11% and myeloma progression in 23.31% of the pts. Median OS for all pts was 76 months [2-282]. Patients with standard-risk FISH/cytogenetics had median OS of 88 months [2-282], compared to 60 months [2-211] in the high-risk group. A subgroup of pts with 13q- only (assessed by metaphase karyotyping), had an OS of 79 months [3-163].
Conclusions:
In the community setting pts with MM, even with high-risk disease, typically survive more than 5 years. The majority (over 66%) die from non-MM-related causes. This observation emphasizes the importance of recognizing comorbidities and utilizing multidisciplinary care for pts with this malignancy.
