Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
Patterns of Use of Free Light Chain Testing in Patients with Multiple Myeloma in Colombia
(PA-526) Patterns of Use of Free Light Chain Testing in Patients with Multiple Myeloma in Colombia

Nohemi Caballero, MD MSc (she/her/hers)
Scientific Affairs Specialist
The Binding Site LATAM, Part of Thermo Fisher Scientific
Introduction:
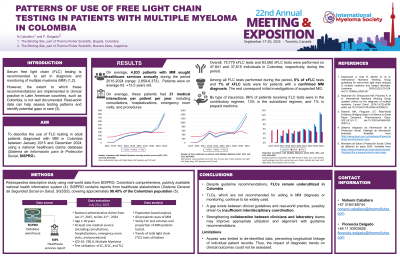
Serum free light chain (FLC) assay is recommended for diagnosis and monitoring of multiple myeloma (MM). However, the extent to which these recommendations are implemented in clinical practice in Latin American countries, such as Colombia, is not well documented. Real-world data can help assess testing patterns and identify potential gaps in care. This study aimed to describe the use of FLC testing in MM patients in Colombia using a national healthcare claims data.
Methods:
We conducted a retrospective, population-based analysis using SISPRO, Colombia’s national health information system, from 2015 to 2024. All individuals aged ≥ 18 years with at least one medical attention (including consultations, hospitalizations, emergency room visits, and procedures) during the period were included. MM cases were identified using ICD-10 codes. Laboratory tests were identified using CUPS codes, Colombia’s standardized procedure classification. We included all prevalent cases of MM and assessed yearly FLC test volumes and proportion of MM patients tested. Trends in the use of total light chain (TLC) test use were analyzed in parallel for comparison.
Results:
Between 2015 and 2024, the yearly number of adult patients attended with a main diagnosis of MM increased from 2,938 to 6,373. The total number of medical attentions for these patients rose from 59,047 in 2015 to 173,707 in 2024. Since 2015, 75,779 κFLC and 63,560 λFLC tests were performed on 47,841 and 37,615 individuals in Colombia, respectively, averaging 1.54 and 1.57 tests per patient per year. When considering all FLC tests, regardless of the associated diagnosis, the number of individuals tested annually increased, from 3 in 2015 to 18,741 in 2024 for κFLC, and from 3 in 2015 to 11,080 in 2024 for λFLC. Among all FLC tests, 6% (κFLC) and 7% (λFLC) were related to an MM diagnosis. The proportion of MM patients attended each year who received at least one FLC test increased during the period, reaching 13.1% for κFLC and 12.3% for λFLC by 2024. Despite the increase in FLC utilization, TLC testing remained in use, increasing from 3,937 total tests in 2015 to 10,141 in 2024. Among all TLC tests performed, 8% were associated with an MM diagnosis. The annual proportion of MM patients receiving at least one TLC test remained relatively stable, ranging from 4.7% to 5.8% during the period.
Conclusions:
Despite guideline recommendations, FLCs remain underutilized in Colombia, whereas TLCs, which are not recommended for MM diagnosis or monitoring, continue to be widely used. This indicates a gap between clinical guidelines and real-world practice, possibly driven by insufficient interdisciplinary coordination. Strengthening collaboration between clinicians and laboratory teams may improve appropriate utilization and alignment with guidelines’ recommendations.
