Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
EVOLUTION OF AGE AND CAUSES OF DEATH IN PATIENTS WITH MULTIPLE MYELOMA IN THE ERA OF NOVEL AGENTS.
(PA-521) Evolution of Age and Causes of Death in Patients with Multiple Myeloma in the Era of Novel Agents

Abel Rosado Rodriguez, Sr. (he/him/his)
MIR Hematología
Hospital of Jerez de la Frontera
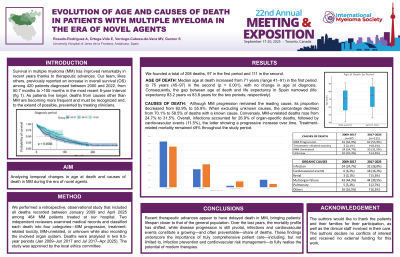
Introduction: Survival in multiple myeloma (MM) has improved markedly in recent years thanks to therapeutic advances. Our group previously reported an increase in overall survival (OS) among 420 patients diagnosed between 2000 and 2022, from 50.7 months to >100 months in the most recent 8-year interval. As patients live longer, deaths from causes other than MM are becoming more frequent and must be recognised and, where possible, prevented by treating clinicians.
Objective: To analyse temporal changes in age at death and causes of death in MM during the era of novel agents.
Methods: We performed a retrospective, observational study that included all deaths recorded between January 2009 and April 2025 among 464 MM patients treated at our centre. Two independent reviewers examined medical records and classified each death into four categories—MM progression, treatment-related toxicity, MM-unrelated, or unknown while also recording the involved organ system. Deaths were analysed in two 8.5-year periods (Jan 2009–Jun 2017 and Jul 2017–Apr 2025). The study was approved by the local ethics committee.
Results: Median age at death increased from 71 years (range 41–91) in the first period to 75 years (45–97) in the second (p = 0.001), with no change in age at diagnosis. Consequently, the gap between age at death and life expectancy in Spain narrowed (life expectancy 83.2 years vs 83.8 years for the two periods, respectively). Causes of death are summarised in Table 1. Although MM progression remained the leading cause, its proportion fell from 70.1 % to 58.5 % of deaths with a known cause. Conversely, MM-unrelated deaths rose from 27.6 % to 33 %. Overall, infections accounted for 26.9 % of organ-specific deaths, followed by cardiovascular events (11.5 %), the latter showing a progressive increase over time. Treatment-related mortality remained ≤9 % throughout the study period.
Conclusions: Recent therapeutic advances appear to have delayed death in MM, bringing patients’ lifespan closer to that of the general population. Over the last years, the mortality profile has shifted: while disease progression is still pivotal, infections and cardiovascular events constitute a growing—and often preventable—share of deaths. These findings underscore the importance of truly comprehensive patient care—including, but not limited to, infection prevention and cardiovascular risk management—to fully realise the potential of modern therapies.
