Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
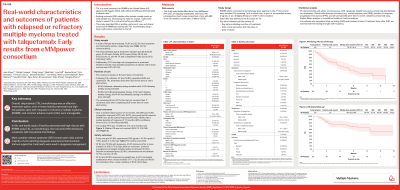
Real-world characteristics and outcomes of patients with relapsed or refractory multiple myeloma treated with talquetamab: Early results from eMMpower consortium
(PA-515) Real-world Characteristics and Outcomes of Patients with Relapsed or Refractory Multiple Myeloma Treated with Talquetamab: Early Results from eMMpower Consortium

Jack Khouri, MD
Associate Professor of Medicine
Cleveland Clinic
Introduction:
Talquetamab (TAL) is a novel treatment for relapsed or refractory multiple myeloma (RRMM) (US approval: 9 Aug 2023). The efficacy and safety of TAL were demonstrated in clinical trials (e.g., MonumenTAL-1). Existing real-world (RW) studies tend to include a single center or a small sample size. To address this evidence gap, this study described RW patient profiles, patterns of care, and clinical outcomes of patients treated with TAL using a large, multi-center consortium in the US.
Methods:
This study used data from eMMpower, a large, ongoing, longitudinal, multi-center chart review consortium for MM (data cutoff date: 31 March 2025). Adults with confirmed MM receiving TAL monotherapy on or after the US approval date were included. Patients receiving TAL as bridging therapy for CAR-T, in a clinical trial, in an expanded access program, or as a combination regimen were excluded.
Results:
A total of 85 patients were included, 76.5% and 23.5% from academic and community centers, respectively. The mean (median) age at treatment initiation was 65.6 (65.9) years; 37.6% were female and 82.4% were White. There were 29.4% with ECOG score ≥2, 14.1%, 27.1%, 36.5% and 22.4% with R-ISS stages I, II, III and unknown, respectively, and 44.7% with a Simplified Frailty Score indicating frailty. Additionally, 67.1% had high-risk cytogenetics and at treatment initiation, 45.9% had bone marrow monoclonal plasma cells ≥60%. Patients received a median of 6 (IQR: 5.0, 7.0) prior lines of therapy.
A total of 67 patients (78.8%) received a treatment dose after step-up dosing, 80.6% having 0.8mg/kg biweekly (Q2W). Over a median follow-up time of 4.1 months, the ORR was 75.6% (≥CR rate: 19.2%; VGPR rate: 29.5%; PR rate: 26.9%) with a median duration of response of 7.5 months. The median PFS was 7.9 (95% CI: 5.3, 10.1) months, while the median OS was not reached. A total of 49 patients (57.6%) experienced cytokine release syndrome (CRS, 43.5% grade 1, 11.8% grade 2, 2.4% grade 3). 43 patients (50.6%) experienced weight loss, of which 19 (44.2%) had weight stabilization after a mean (median) of 77.7 (32.0) days, and 8 (18.6%) had resolution after a mean (median) of 95.0 (34.0) days. Among 62 patients (72.9%) with dysgeusia, 45.2% had improvement after a mean (median) of 105.0 (78.5) days while on treatment. Common dysgeusia management strategies included saline mouthwash (43.5%), biotene mouthwash/spray (30.6%), dexamethasone mouthwash (17.7%), and zinc (11.3%).
Conclusions:
In this real-world study of heavily pretreated and high-risk patients with RRMM using TAL as monotherapy, the real-world effectiveness is consistent with the pivotal trial findings. Most CRS events were mild, and the majority of patients reporting dysgeusia experienced improvement. Various supportive treatments were used in dysgeusia management. Overall, TAL was an effective treatment option even in these heavily pretreated and high-risk patients with RRMM and common AEs were manageable.
