Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Real-World Management of Relapsed/Refractory Multiple Myeloma Following Early Anti-CD38 Exposure
(PA-528) Real-World Management of Relapsed/Refractory Multiple Myeloma Following Early Anti-CD38 Exposure

Esther Ortega, MD (she/her/hers)
Hematology consultant at Jerez de la Frontera Hospital
Hospital Universitario Jerez de la Frontera
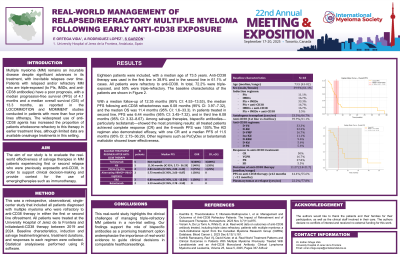
Introduction: Multiple myeloma (MM) remains an incurable disease despite significant advances in its treatment, with inevitable relapses over time. Patients with relapsed and/or refractory MM who are triple-exposed (to PIs, IMiDs, and anti-CD38 antibodies) have a poor prognosis, with a median progression-free survival (PFS) of 4.1 months and a median overall survival (OS) of 13.3 months, as reported in the LOCOMMOTION and MOMMENT studies conducted in patients with more than four prior lines of therapy. The widespread use of anti-CD38 agents has increased the proportion of patients who become refractory to this therapy in earlier treatment lines, although limited data are available on salvage treatments in this setting. The aim of our study is to evaluate the real-world effectiveness of salvage therapies in MM patients experiencing first or second relapse who were previously exposed to anti-CD38, in order to support clinical decision-making and provide context for the use of emerging therapies such as immunotherapy.
Methods:
This was a retrospective, observational, single-center study that included all patients diagnosed with multiple myeloma who were refractory to anti-CD38 therapy in either the first or second line of treatment. All patients were treated at the University Hospital of Jerez de la Frontera and initiated anti-CD38 therapy between 2019 and 2024. Baseline characteristics, induction and salvage treatment regimens, treatment durations, and responses to each regimen were collected. Statistical analysis was performed using R software.
Results: Eighteen patients were included, with a median age of 73.5 years. Anti-CD38 therapy was used in the first line in 38.9% and in the second line in 61.1% of cases. All patients were refractory to anti-CD38. In total, 72.2% were triple-exposed, and 50% were triple-refractory.
With a median follow-up of 12.35 months (95% CI: 4.53–13.53), the median PFS following anti-CD38 refractoriness was 6.08 months (95% CI: 3.97–7.32), and the median OS was 11.4 months (95% CI: 1.6–33.3). In patients treated in second line, PFS was 6.44 months (95% CI: 3.45–7.32), and in third line 6.08 months (95% CI: 3.32–8.67). Among salvage therapies, bispecific antibodies—particularly teclistamab—showed the most promising results: all treated patients achieved complete response (CR) and the 6-month PFS was 100%. The KD regimen also demonstrated efficacy, with one CR and a median PFS of 11.5 months (95% CI: 2.73–36.29). Other regimens such as PoCyDex or belantamab mafodotin showed lower effectiveness.
Conclusions: This real-world study highlights the clinical challenges of managing triple-refractory MM patients in a non-trial setting. Our findings support the role of bispecific antibodies as a promising treatment option and emphasize the importance of real-world evidence to guide clinical decisions in comparable healthcare settings. Additional figures, survival curves, and detailed data will be presented in the final poster.
