Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
Infectious Complications in Patients with Multiple Myeloma: A Scoping Review
(PA-148) Infectious Complications in Patients with Multiple Myeloma: A Scoping Review
.jpeg.jpg)
Aditi Raghav, MBBS (pursuing)
Student
Army College of Medical Sciences
Introduction:
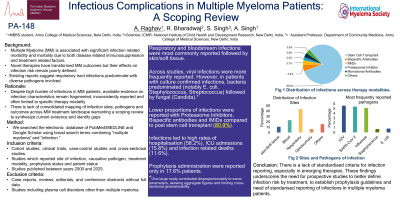
Multiple Myeloma (MM) patients face heightened infection risks due to disease-related immunosuppression and therapies. Emerging data suggest that novel immunotherapies (bispecific antibodies, CAR-T) may further alter infection profile in patients, but evidence remains fragmented. This scoping review aims to map existing literature on characteristics and outcomes of infections in MM patients and highlight key gaps.
Methods:
We searched PubMed/MEDLINE and Google Scholar using broad search terms combining “multiple myeloma” and “infection.” Studies published between 2000 and 2025 were considered, with the final search conducted on 6th May 2025. Eligible studies included those that reported both the site of infection and the identified pathogen in patients with multiple myeloma. Case reports, reviews, editorials, and conference abstracts without full data were excluded. A total of 21 studies met the inclusion criteria. Data was collected and organized in Microsoft Excel, and synthesized descriptively through tabulation and frequency analysis to highlight common patterns and trends across studies.
Results:
A total of 7,442 MM patients with infections were identified. Median age ranged from 56–72 years (17 studies); other three studies reported mean values and one reported average value. 13 studies reported ISS staging, with 4,624 patients (63.9%) in stages I–II and 2,613 patients (36.1%) in stage III. Among 20 studies, 4,501 (42.8%) were female and 5,995 (57.2%) male. IgG subtype was most common (95.1%), followed by IgA (2.7%) and light chain (1.9%). Infections were highest post-stem cell transplant (80.9%), followed by bispecific antibodies (5.2%) and IMiDs (3.7%). Of 9,403 reported infection sites, respiratory (43.6%) was most common, followed by bloodstream (23.7%) and skin/soft tissue (10.7%). Bacteria predominated, followed by viruses and fungi. Frequently reported pathogens included E. coli , Staphylococcus, Streptococcus, VZV, SARS-CoV-2, influenza, and Candida species. Despite the infection burden, only 1,281 (17.21%) patients were reported to have received prophylaxis, suggesting limited use or under reporting. 745 (58.2%) hospitalizations were reported across 13 studies, 125 (15.8%) ICU admissions in 8 studies, and 1,481 (11.6%) infection-related deaths in 18 studies. It is important to note that one large study contributed disproportionately to some parameters, skewing aggregate figures and limiting cross-study generalizability, high incidence of viral infections can be influenced due to COVID-19 infections.
Conclusions:
There is a lack of standardized criteria for infection reporting, especially in emerging therapies such as CAR-T and bispecific antibodies. These findings highlight the need for prospective studies to better define infection risk by treatment, establish prophylaxis guidelines, assess outcomes in underrepresented subgroups and need of standardized reporting of infections.
