Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Category: Treatment of Newly Diagnosed Myeloma (excluding t-cell redirection therapy)
Definition of transplant ineligibility in newly diagnosed multiple myeloma: a systematic review
(PA-415) Definition of Transplant Ineligibility in Newly Diagnosed Multiple Myeloma: A Systematic Review

Karun Neupane, MD (he/him/his)
Hematology Oncology Fellow
Moffitt Cancer Center
Methods:
This study built on a previously published systematic review, the protocol for which is registered on Open Science Framework. We included phase II and III RCTs that exclusively enrolled transplant-ineligible NDMM patients published through October 2023. For each study, we collected data on reported criteria for transplant ineligibility and patient characteristics in the main manuscript and/or protocol/supplement.
Results:
Of 264 identified RCTs, 50 (19%) exclusively enrolled transplant-ineligible patients (88% available as full manuscripts). Study protocols and supplementary data allowing for detailed analysis of enrollment criteria were available for 32 studies (64%).
Among 50 transplant-ineligible trials, only 22 (44%) explicitly defined ineligibility criteria. Of these, 20 (40%) trials used age as a cut-off with/without other criteria including: age alone (n=1, 2%), combination of age/comorbidities (n=15, 30%), age/comorbidities/personal preference (n=2, 4%), age/significant comorbidities/insufficient stem cells/patient preference (n=1, 2%), and age/no access due to cost or other reasons/patient preference (n=1, 2%) . The remaining two trials (4%) used investigator judgment (n=1, 2%), and comorbidities/patient preference (n=1, 2%). Notably, only two studies explicitly specified which comorbidities constituted transplant ineligibility.
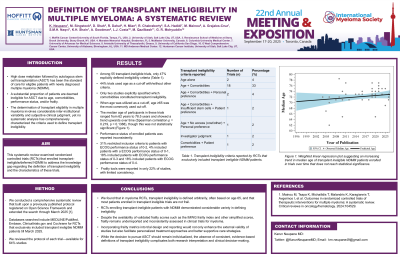
All trials using age cut-offs for transplant ineligibility (n=20, 40%) uniformly applied a threshold of ≥65 years. The median age of participants in these trials ranged from 62 years to 78.5 years, with an increasing trend over time (p=0.003). While 58% of trials reported ECOG or Karnofsky performance status, none utilized these scores as formal criteria for transplant ineligibility. Among a total of 14 trials (28%) that reported enrolling patients with ECOG 3-4, these patients represented 1-26% of enrolled patients. Standardized frailty tools were employed in 24% of studies (IMWG 16%, simplified frailty score 8%).
Conclusions: RCTs enrolling transplant-ineligible patients with NDMM demonstrated considerable variety in defining ineligibility. This heterogeneity in eligibility criteria has important implications for interpreting trial results and clinical practice. While the decision to pursue transplantation should remain individualized, the absence of consistent, evidence-based definitions of transplant ineligibility complicates both research interpretation and clinical decision-making.
