Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
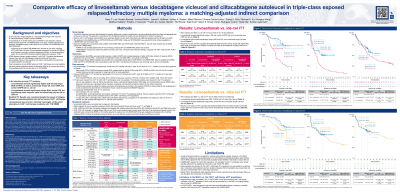
Comparative efficacy of linvoseltamab versus idecabtagene vicleucel and ciltacabtagene autoleucel in triple-class exposed relapsed/refractory multiple myeloma: a matching-adjusted indirect comparison
(PA-050) Comparative Efficacy of Linvoseltamab versus Idecabtagene Vicleucel and Ciltacabtagene Autoleucel in Triple-class Exposed Relapsed/refractory Multiple Myeloma: A Matching-adjusted Indirect Comparison

Hans C. Lee, MD
Director, Multiple Myeloma Research
Sarah Cannon Research Institute
Direct comparisons of anti–B-cell maturation antigen (BCMA) bispecific antibodies and chimeric antigen receptor T cell (CAR-T) therapies are lacking in triple-class exposed (TCE) relapsed/refractory multiple myeloma (RRMM). We used matching-adjusted indirect comparisons (MAICs) to compare linvoseltamab (linvo) with idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel), using intention-to-treat (ITT: enrolled, apheresed, bridging therapy if applicable) and modified ITT (mITT: infused) populations from CAR-T trials.
Methods:
Patient (pt)-level data from LINKER-MM1 (linvo; ITT/mITT 117 pts; data cut-off [DCO] 7/24; median follow-up [mFU] 21.3 months [mos]) and published data from KarMMa (ide-cel; ITT 149, mITT 137; DCO 12/23; mFU 63.6 mos) and CARTITUDE-1 (cilta-cel; ITT 113, mITT 97; DCO 10/22; mFU 33.4 mos) were used. To align with CAR-T trial eligibility, LINKER-MM1 pts with prior BCMA antibody–drug conjugates (all analyses) and pts not refractory to their last line (ide-cel analyses only) were excluded. Unavailable ITT data for CAR-T trials were imputed from mITT populations. Outcome definitions were harmonized where possible. LINKER-MM1 pts were weighted to match each CAR-T trial on pre-specified key prognostic factors. Outcomes included objective response rate (ORR), very good partial response or better (≥VGPR) and complete response or better (≥CR) rates, duration of response (DOR), progression-free (PFS) and overall survival (OS).
Results:
After matching, vs ide-cel ITT (effective sample size [ESS] 43.7), linvo had significantly higher ≥CR rate (OR 1.83, 95% CI 1.12–3.01), similar ≥VGPR rate (OR 0.93, 0.57–1.51), and significantly longer DOR (HR 0.21, 0.10–0.44) and PFS (HR 0.52, 0.29–0.91). Although not significant, linvo had lower ORR (OR 0.67, 0.40–1.15) and longer OS (HR 0.77, 0.44–1.35). Results vs ide-cel mITT (43.9) were similar to those in the ITT, with significantly lower ORR and numerically lower ≥VGPR and higher ≥CR rates with linvo.
Vs cilta-cel ITT (52.8), linvo had significantly lower ORR (OR 0.41, 0.22–0.76) and ≥VGPR (OR 0.37, 0.21–0.66) and ≥CR rates (OR 0.40, 0.24–0.66), but longer DOR (HR 0.46, 0.22–0.95). PFS was similar (HR 1.08, 0.62–1.91) and, though not significant, OS was shorter (HR 1.27, 0.71–2.25). Results vs cilta-cel mITT (57.6) were similar, with numerically longer DOR and shorter PFS with linvo.
Conclusions:
Linvo showed significantly higher ≥CR rate and longer DOR and PFS, and numerically longer OS vs ide-cel in the ITT population, and numerically lower ORR and similar ≥VGPR rate. Vs cilta-cel ITT, linvo showed significantly longer DOR and similar PFS despite significantly lower response rates and numerically shorter OS. Although outcomes improved in the CAR-T mITT populations and MAIC results were broadly consistent, the impact of bridging therapy on these comparisons remains unclear. These findings suggest linvo has the potential to offer a clinically meaningful, off-the-shelf alternative to CAR-T therapies in TCE RRMM.
