Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
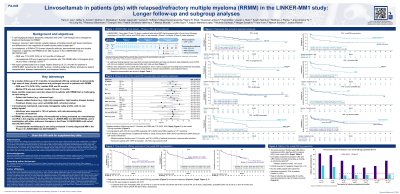
Linvoseltamab in patients (pts) with relapsed/refractory multiple myeloma (RRMM) in the LINKER-MM1 study: longer follow-up and subgroup analyses
(PA-049) Linvoseltamab in Patients (pts) with Relapsed/refractory Multiple Myeloma (RRMM) in the LINKER-MM1 Study: Longer Follow-up and Subgroup Analyses

Hans C. Lee, MD
Director, Multiple Myeloma Research
Sarah Cannon Research Institute
In pts with triple-class exposed RRMM, linvoseltamab (BCMA×CD3 bispecific antibody) demonstrated high response rates, with early responses that deepened over time, and a generally manageable safety profile. Here we report longer-term follow-up of pts receiving the EMA-approved 200 mg dose, including subgroup efficacy analyses by risk status and prior treatment, in the Phase (Ph) 1/2 LINKER-MM1 study (NCT03761108).
Methods:
In Ph2, pts received linvoseltamab IV QW through Week 14, then Q2W. Ph2 200 mg pts with ≥VGPR and ≥24 weeks of treatment switched to Q4W dosing. Ph2 primary endpoint was objective response rate (ORR) by IRC. Efficacy was assessed in prespecified subgroups defined by age, ISS stage, cytogenetic risk, baseline (BL) sBCMA concentration, BMPC %, EMP, and disease refractoriness; efficacy by prior treatment was analyzed post hoc.
Results:
This analysis included 117 pts: median age, 70 yrs (range 37–91); ISS III, 18%; high-risk cytogenetics, 39%; median sBCMA, 377 ng/mL (165–909); median BMPC, 23% (1–100); EMP, 16%; ≥penta-refractory, 29%. As of Jul 23, 2024, median duration of follow-up was 21.3 mos.
In the overall 200 mg cohort, ORR was 71% (≥CR, 52%) and median duration of response was 29.4 mos (95% CI: 20.0‒not evaluable [NE]). Median progression-free survival was not reached (17.3 mos‒NE) and median overall survival was 31.4 mos (23.8‒NE). From Ph2, 58/105 (55%) pts transitioned to Q4W dosing at ≥24 weeks of treatment. For these 58 pts, total median treatment duration was 12.8 mos, and 43 remained in response after transition. Among 27 pts with VGPR at transition, 19 (70%) later achieved ≥CR.
Response rates were high across subgroups of the overall 200 mg cohort, including by age (≥75 yrs, ORR 71%; ≥65‒< 75 yrs, 76%; < 65 yrs, 66%), ISS stage (I, 73%; II, 71%; III, 62%), cytogenetic risk (high, 67%; standard, 73%), BL sBCMA (≥400 ng/mL, 57%; < 400 ng/mL, 83%), BL BMPC (≥50%, 50%; >0‒< 50%, 79%), and BL EMP (EMP+, 53%; EMP−, 74%), and in pts with penta-refractory disease (68%).
ORR was 72% (64/89) in pts with ≥4 prior LoT and 70% (7/10) in pts with prior anti-BCMA antibody-drug conjugate (belantamab mafodotin) exposure. Time-to-event outcomes by subgroup will be presented.
Treatment-emergent AEs (TEAEs) occurred in all pts (Grade [Gr] ≥3, 88%). No new safety signals were observed. In total, 21% of pts discontinued due to TEAEs. The most common TEAEs were CRS (any Gr 46%), neutropenia (44%), diarrhea (42%), anemia, and cough (both 40%). Infections occurred in 75% (Gr 3–4 37%) of pts, with rate decreasing after 6 mos of treatment (0–< 3 mos: any Gr 52%/Gr 3–4 21%; 3–< 6 mos: 49%/22%; 6–< 9 mos: 37%/6%; 9–< 21 mos [in each 3-mo period]: 23–37%/0–8%).
Conclusions:
This longer-term analysis showed that linvoseltamab 200 mg induced high rates of deep, durable response and prolonged survival in pts with RRMM, including those with heavily pretreated and high-risk disease, while maintaining a generally manageable and consistent safety profile.
