Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
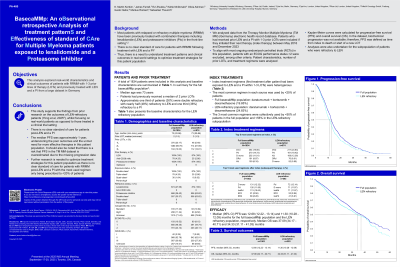
BASECAMMP: An OBservational Retrospective Analysis of Treatment PatternS and Effectiveness of Standard of CAre for Multiple Myeloma Patients Exposed to Lenalidomide and a Proteasome Inhibitor
(PA-480) BASECAMMP: An OBservational Retrospective Analysis of Treatment PatternS and Effectiveness of Standard of CAre for Multiple Myeloma Patients Exposed to Lenalidomide and a Proteasome Inhibitor

K. Martin Kortüm (he/him/his)
Professor
Department of Internal Medicine II, University Hospital of Würzburg
Methods:
We analysed data from the Therapy Monitor Multiple Myeloma (TM MM) (Germany) electronic health record database. Patients who had previously received LEN and a PI with 1-3 prior LOTs were included if they initiated their next therapy (index therapy) between May 2016 and December 2023. To align with most ongoing randomized-controlled trials (RCTs) in this population, patients with an ECOG PS >2 were excluded, among other criteria. Patient characteristics, number of prior LOT, and treatment regimens were analyzed. Kaplan-Meier curves were calculated for progression-free survival (PFS) and overall survival (OS). In the TM MM dataset, biochemical progression was not available, therefore PFS was defined as time from index to death or start of a new LOT.
Results:
A total of 1834 patients were included in this analysis. The median age was 73 years and 41% of patients were female. Patients had received a median of 2 prior LOTs. Approximately a third of patients (30%) were double refractory with nearly half (48%) refractory to LEN and a third (36%) refractory to a PI. Index treatment regimens were heterogeneous. The 3 most common regimens were collectively used by < 50% of patients (daratumumab + bortezomib + dexamethasone [19.9%], pomalidomide + dexamethasone [14.7%], daratumumab monotherapy [11.0%]). The median PFS (95% CI) was 12.7 months (12.2-13.1) and median OS was 37.1 months (34.2-40.7). The results were very similar for the lenalidomide refractory population (n=847) who had a median PFS of 11.3 months (10.3-12.1) and a median OS of 34.3 months (31.1-41.0).
Conclusions:
The median PFS was approximately one year, highlighting the poor outcomes and an unmet need for more effective therapies in this patient population. It should also be noted that there is a risk that the median PFS was overestimated due to the missing progression data.
Further research is needed to optimize treatment strategies for this patient population as there is no clear standard of care for patients with RRMM post-LEN and a PI with the most used regimen only being prescribed to less than 20% of patients.
