Nursing and Allied Health Symposium
Category: Nursing & Allied Health Symposium
Bispecific Antibody Therapy in Haematology: A National Cancer Nurse Education Needs Assessment in the United Kingdom
(NSP-05) Bispecific Antibody Therapy in Haematology: A National Cancer Nurse Education Needs Assessment in the United Kingdom

Chantelle Hughes, RN, MNursSci (she/her/hers)
Senior Research Nurse
University College London Hosptial
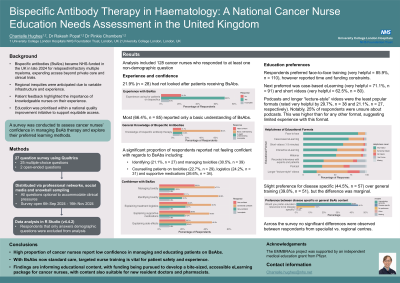
Bispecific antibodies (BsAbs) were funded in the UK for patients with relapsed/refractory multiple myeloma in late 2024, offering a promising new treatment option. However, regional inequities in access were anticipated due to variable levels of experience and infrastructure. Patient feedback highlighted the importance of knowledgeable nurses in their understanding and experience of treatment.
As a result, education was prioritised within a national quality improvement initiative. To inform this, we developed a survey to assess cancer nurses’ confidence in managing BsAb therapy and to explore their preferred learning methods.
Methods:
We developed a 27-question survey (25 multiple-choice, 2 open-ended) using the platform Qualtrics. To accommodate clinical pressures, all questions were optional. The survey was distributed through professional networks, social media, and snowball sampling. Data were analysed using R Studio (v4.4.2).
Results:
149 nurses responded from across the UK. Respondents represented a range of hospital types (specialist 56% (n=83), regional 42% (n=62)) and roles (nurse specialists 33% (n=49), ward/daycare nurses 31% (n=46), research nurses 11% (n=17), nurse practitioners 7% (n=11), other 17% (n=25)).
Overall, confidence in managing BsAbs was low. Only 17% (n=25) felt very confident identifying BsAb-related toxicities, while 44% (n=65) were somewhat confident and 18% (n=24) not confident. Confidence in managing toxicities was even lower, with just 11% (n=17) very confident, 41% (n=61) somewhat confident, and 26% (n=39) not confident. Confidence levels did not differ significantly between nurses in specialist and regional hospitals for identifying (χ² = 0.65, p = 0.72) and managing toxicities (χ² = 2.31, p = 0.32).
Confidence in counselling patients about supportive medications was also limited: 23% (n=34) were not confident, 27% (n=55) somewhat confident, and 19% (n=28) confident. Similarly when discussing potential side effects, 20% (n=30) felt very confident, 39% (n=58) somewhat confident and 20% (n=29) not confident. No significant differences were observed between hospital types for counselling on expected toxicities (χ² = 1.33, p = 0.51) or supportive medicines (χ² = 0.02, p = 0.99). Nurse specialists reported the highest confidence across all domains, while other roles showed notably lower levels.
In-person training was the preferred educational format, with 74.3% (n=110) rating it as very helpful, though respondents reported challenges attending due to time and funding constraints. Case-based eLearning and short videos were the next favoured formats, with 61.5% (n=91) and 54.1% (n=80) respectively rating them as very helpful, indicating they may offer acceptable more accessible alternatives.
Conclusions:
This national survey highlights low confidence among cancer nurses in managing and educating patients on BsAbs. As these therapies are now standard of care, tailored nurse training is essential to ensure patient safety and enhance patient experience.
