Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Real-World Comparison of Idecabtagene Vicleucel and Ciltacabtagene Autoleucel in Relapsed/Refractory Multiple Myeloma: A Center for International Blood & Marrow Transplantation Research (CIBMTR) Study
(PA-003) Real-World Comparison of Idecabtagene Vicleucel and Ciltacabtagene Autoleucel in Relapsed/Refractory Multiple Myeloma: A Center for International Blood & Marrow Transplantation Research (CIBMTR) Study
.jpg)
Aimaz Afrough, MD (she/her/hers)
Assistant Professor
Hematologic Malignancies and Cellular Therapy Program, Simmons Comprehensive Cancer Center, University of Texas Southwestern Medical Center
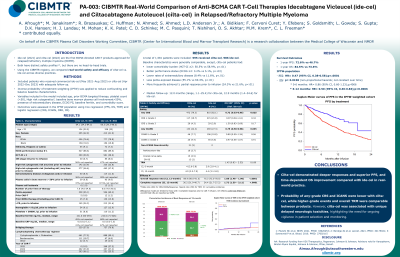
Idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel) are BCMA CAR-T products approved for relapsed/refractory multiple myeloma in 2021 and 2022, respectively, with distinct safety profiles. In the absence of head-to-head trials, we used CIBMTR data to compare their safety and efficacy in a real-world setting.
Methods:
We included patients (pts) who received commercial ide-cel (May 2021–Aug 2023) or cilta-cel (Apr 2022–Dec 2023) with adequate follow-up. To reduce confounding and balance baseline characteristics, we used inverse probability of treatment weighting (IPTW) based on propensity score model. Multivariable analysis was conducted using logistic and Cox regression models.
Results:
Of 1581 pts, 595 received cilta-cel and 986 ide-cel. Baseline characteristics were generally comparable, except cilta-cel cohort had lower comorbidity burden (HCT-CI ≥2: 50.5% vs 58.9%, p< .01), better performance status (ECOG ≥2: 3.2% vs 5.1%, p=.03), fewer with extramedullary disease (8.4% vs 11.6%, p< .01), and less penta-exposed disease (55.1% vs 60.4%, p< .01), while a greater proportion achieved ≥ partial response at infusion (24.3% vs 21.6%, p< .01). Median follow-up of survivors was 12.0 months (range, 1.1–25.4) for cilta-cel, and 12.9 months (range, 1.4–34.6) for ide-cel.
Any grade CRS occurred in 79.3% vs 82.1%, and grade ≥3 in 4.3% vs 2.9% (cilta-cel vs ide-cel). Any grade ICANS was seen in 22.3% vs 27.3%, and 6-month treatment-related mortality (TRM) was 4.0% (95% CI, 2.6–5.8) vs 2.9% (95% CI, 2.0–4.1), respectively. After IPTW adjustment, cilta-cel remained associated with lower odds of any grade CRS [odds ratio (OR), 0.72, p=.0004)], and any grade ICANS (OR 0.75, p=.0005), but higher odds of grade ≥3 CRS (OR 1.50, p=.041), with no difference in grade ≥3 ICANS (OR 0.97, p=.8). In the unadjusted cilta-cel cohort, 5% had non-ICANS neurologic events—Parkinsonism (2.7%) and cranial nerve palsies (2.5%), most commonly involving the facial nerve (12/15); no such events were reported with ide-cel.
At 12 months, cumulative incidence of overall response rate (ORR) and complete response (CR) was higher in cilta-cel (ORR: 88.9% vs 75.3%; CR: 36.2% vs 24.4%). One-year progression-free survival (PFS) was 72.6% vs 46.7%, and overall survival (OS) was 84.5% vs 73.6% (cilta-cel vs ide-cel). After IPTW adjustment, cilta-cel remained associated with higher odds of ORR (OR 1.7; 95% CI, 1.56–1.84; p< .0001) and CR (OR 1.88; 95% CI, 1.66–2.14; p< .0001), and longer PFS [hazard ratio (HR) 0.47; 95% CI, 0.41–0.53; p< .0001] and OS (HR 0.82; 95% CI, 0.70–0.95; p=.008). However, TRM was higher with cilta-cel (HR 1.45; 95% CI, 1.06–1.98; p=.018).
Conclusions: In this largest real-world comparison to date, cilta-cel showed deeper responses and improved PFS/OS, but was associated with more delayed neurotoxicity and higher TRM—highlighting the need for optimized patient selection and proactive risk mitigation strategies.
*AA & MJ contributed equally
