Cellular and T cell engager Immunotherapy
Category: Cellular and T cell engager Immunotherapy
Clonal hematopoiesis of indeterminate potential (CHIP) does not impact the efficacy of BCMA-directed chimeric antigen receptor (CAR)-T cells in patients with relapsed/refractory multiple myeloma
(PA-012) Clonal Hematopoiesis of Indeterminate Potential (CHIP) Does Not Impact the Efficacy of BCMA Directed Chimeric Antigen Receptor (CAR)-T Cells in Patients with Relapsed/refractory Multiple Myeloma

Sophie G. Carlson, MD
Fellow Physician
UCLA
Introduction:
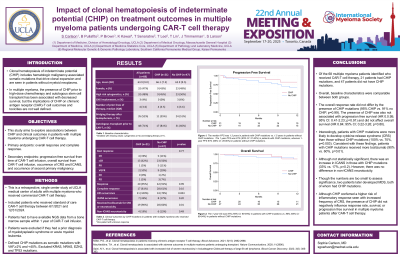
Clonal hematopoiesis of indeterminate potential (CHIP) is the presence of hematologic malignancy-associated somatic mutations that drive hematopoietic stem cell clonal expansion and are seen in patients without hematologic malignancies. In multiple myeloma (MM), the implications of CHIP on chimeric antigen receptor (CAR)-T cell outcomes and toxicities have yet to be fully explored. This study aims to investigate associations between CHIP and clinical outcomes in patients with MM undergoing CAR-T cell therapy.
Methods:
We performed a retrospective, single center study at UCLA Medical Center of adults with multiple myeloma who received commercial CAR-T cell therapy from 6/1/2021 to 12/31/2024. Patients were required to have NGS data from a bone marrow sample within 1 year prior to CAR-T cell infusion. Patients were excluded if they had a prior diagnosis of myelodysplastic syndrome or acute myeloid leukemia. CHIP mutations were defined as somatic mutations with VAF >=2% and < 40%, and KRAS, NRAS, EZH2, and TP53 mutations were excluded.
Results:
Of the 68 adult patients identified, 21 (31%) patients had CHIP mutations. The mean age was comparable between groups at 63 years old without CHIP and 66 years old with CHIP. The median number of prior lines of therapy in both groups was 4 (ranges 2 to 11), and the presence of high-risk cytogenetics was similar between groups (45% with CHIP vs. 50% no CHIP). A single CHIP mutation was detected in 15/21 patients, while six patients had two or more mutations in different genes with DNMT3A as the most common mutation. The overall response rate (95% in CHIP vs. 91% in no CHIP; p=0.99) and the complete response rate did not differ by CHIP status (81% in CHIP vs. 61% in no CHIP; p=0.10). Similarly, CHIP mutations did not impact progression free survival (PFS of 1.3 years in patients with CHIP mutations vs. 1.5 years without CHIP mutations;HR 0.95; 95% CI: 0.41-2.23; p=0.91) nor overall survival with a 1-year OS of 87% (95% CI: 69-94%) in patients with CHIP mutations vs. 86% (95% CI: 69-94%) in patients without CHIP mutations (HR 0.84; 95% CI; 0.22-3.26; p=0.80). Patients with CHIP mutations were more likely to develop CRS (100% vs. 70%; p=0.007) and to receive tocilizumab for CRS (90% vs. 60%; p=0.01) than patients without CHIP mutations; however, there was no difference in the incidence of ICANS (33% in patients with CHIP vs. 17% in patients without CHIP, p=0.20). While there was no difference in cytopenias at days 90 or 120, there was a notable increase in the amount of G-CSF used between days 90-120 (27.8% in CHIP vs. 5% without CHIP, p=0.02).
Conclusions:
Although CHIP did not negatively influence the response rate, complete response rate, survival, or progression free survival in MM patients after CAR-T cell therapy, it did confer a higher risk of inflammatory response seen with increased frequency and grade of CRS.
