Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Real-world evidence of melflufen plus dexamethasone in heavily pretreated relapsed/refractory multiple myeloma patients: efficacy and safety from a single-center experience.
(PA-487) Real-world Evidence of Melflufen Plus Dexamethasone in Heavily Pretreated Relapsed/refractory Multiple Myeloma Patients: Efficacy and Safety from a Single-center Experience

Katia Mancuso, katia.mancuso (she/her/hers)
Hematologist and Junior Assistant Professor
Università di Bologna - IRCCS Azienda Ospedaliero-Universitaria di Bologna, Istituto di Ematologia "Seràgnoli"
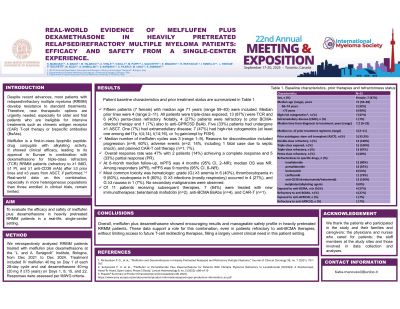
Despite recent advances, most patients with relapsed/refractory multiple myeloma (RRMM) develop resistance to standard treatments. Therefore, new therapeutic options are urgently needed, especially for older and frail patients who are ineligible for intensive treatments such as chimeric antigen receptor (CAR) T-cell therapy or bispecific antibodies (BsAbs). Melflufen is a first-in-class lipophilic peptide-drug conjugate with alkylating activity. It showed clinical efficacy, leading to its approval in Europe in combination with dexamethasone for triple-class refractory (TCR) RRMM patients (refractory to ≥1 IMiD, ≥1 PI, and ≥1 anti-CD38 mAb) after ≥3 prior lines and ≥3 years from ASCT, if performed. Real-world data on this combination, especially in more heterogeneous populations than those enrolled in clinical trials, remain limited.
Methods:
We retrospectively analyzed RRMM patients treated with melflufen plus dexamethasone at the “L. and A. Seràgnoli” Institute, Bologna, from Dec 2021 to Dec 2024. Treatment included IV melflufen 40 mg on Day 1 of each 28-day cycle and oral dexamethasone 40 mg (20 mg if ≥75 years) on Days 1, 8, 15, and 22. Responses were assessed per IMWG criteria.
Results:
Fifteen patients (7 female) with median age 71 years (range 59–83) were included. Median prior lines were 4 (range 2–11). All patients were triple-class exposed; 13 (87%) were TCR and 6 (40%) penta-class refractory. Notably, 5 (33%) patients were refractory to prior BCMA-directed therapy and 1 (7%) also to anti-GPRC5D BsAb. Five (33%) patients had undergone ≥1 ASCT. One (7%) had extramedullary disease; 4 (27%) had high-risk cytogenetics (at least one among del17p, t(4;14), t(14;16), or 1q gain/ampl by FISH).
Median number of melflufen cycles was 3 (range 1–9). Reasons for discontinuation included progression (n=9; 60%), adverse events (n=2; 14%, including 1 fatal case due to septic shock), and planned CAR-T cell therapy (n=1; 7%). Overall response rate was 47% with 2 patients (14%) achieving a complete response and 5 (33%) partial response (PR). At 8-month median follow-up, mPFS was 4 months (95% CI, 2–NR); median OS was NR. Among responders (≥PR), mPFS was 9 months (95% CI, 8–NR). Most common toxicity was hematologic: grade (G) ≥3 anemia in 6 (40%), thrombocytopenia in 9 (60%), neutropenia in 9 (60%). G ≥3 infections (mostly respiratory) occurred in 4 (27%), and G ≥3 nausea in 1 (7%). No secondary malignancies were observed. Of 11 patients receiving subsequent therapies, 7 (64%) were treated with new immunotherapies: belantamab mafodotin (n=2), anti-BCMA BsAbs (n=4), and CAR-T (n=1).
Conclusions:
Overall, melflufen plus dexamethasone showed encouraging results and manageable safety profile in heavily pretreated RRMM patients. These data support a role for this combination, even in patients refractory to anti-BCMA therapies, without limiting access to future T-cell redirecting therapies, filling a largely unmet clinical need in this patient setting.
