Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Category: Treatment of Relapsed/Refractory Myeloma (excluding T-cell redirection therapy)
Socioeconomic factors affecting health equity in patients with relapsed or refractory multiple myeloma (RRMM)
(PA-481) Socioeconomic Factors Affecting Health Equity in Patients with Relapsed or Refractory Multiple Myeloma (RRMM)

Yvonne A. Efebera, MD, MPH
Medical Director - Blood and Marrow Transplant and Cellular Therapy
OhioHealth
Socioeconomic factors impact health equity among patients (pts) with RRMM, often limiting access to advanced treatments (Tx) like CAR-T and bispecific antibodies (BsAbs). Identifying and addressing these determinants may ensure equitable care for all pts with RRMM.
Methods:
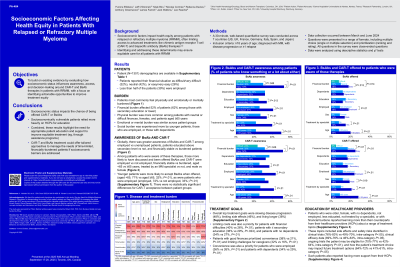
This prospective survey-based study (March-June 2024) included 1301 pts with RRMM and 983 oncologists from 7 countries. Data were analyzed using descriptive statistics and χ2 tests; only pt data are reported. P<.01 was used for all comparisons, unless specified.
Results:
Financial burden affected 52% of pts (62% among those with secondary education or lower). Pts with financial difficulties had worse physical burdens than those in better circumstances (77% vs 61%), and Tx outcomes for them were worse than expected for quality of life, side effects, and mental health. They prioritized limiting costs (40% vs 26%), whereas pts with good finances prioritized convenience (38% vs 21%) and limiting challenges for caregivers (32% vs 16%).
Globally, there was greater awareness of CAR-T and BsAbs among employed vs unemployed pts (CAR-T, 44% vs 29%; BsAb, 41% vs 26%), educated above secondary level vs not (CAR-T, 37% vs 26%, statistically insignificant; BsAb, 34% vs 25%), and financially stable vs burdened (CAR-T, 52% vs 24%; BsAb, 53% vs 16%). Among pts who were aware of these therapies, those more likely to have discussed and been offered CAR-T and BsAbs were employed vs not employed (CAR-T, 24% vs 12%; BsAbs, 18% vs 9%), financially stable vs burdened (CAR-T, 25% vs 5%; BsAbs, 18% vs 8% P=.014), <65 vs ≥65 years (CAR-T, 28% vs 9%; BsAbs, 20% vs 8%), treated by an MM specialist vs not (CAR-T, 21% vs 10%; BsAbs, 15% vs 8%), and male vs female (CAR-T, 19% vs 12%, P=.019; BsAb, 14% vs 9%, stat insig). Younger and employed pts were more likely to accept BsAbs when offered (<65, 71% vs ≥65, 32%; employed, 72% vs not employed, 33%), with statistically insignificant differences for CAR-T acceptance. Expectations were better met for pts who discussed or were offered CAR-T and BsAbs.
Pts who were older, female, with no dependents, unemployed, less educated, not treated by a specialist, or with financial burdens reported learning more than their counterparts from their healthcare providers (HCPs) about a range of Tx topics, including side effects and safety risks identified in clinical trials, clinical efficacy data, ongoing trials the pt may be eligible for, and how the pt’s Tx choice may impact future Tx options. Such pts also reported having more support from their HCPs.
Conclusions:
Socioeconomic status impacts the chance of being offered CAR-T or BsAbs, and socioeconomically vulnerable pts relied more heavily on HCPs for education. Combined, these results highlight the need for appropriate pt education and support to improve equitable Tx (eg, through assistance programs). CAR-T and BsAb Tx could offer tailored approaches to time-limited, financially-burdened pts needs if socioeconomic barriers are addressed.
