Imaging, QoL and Patient-Reported Outcome and Supportive Care
Category: Imaging, QoL and Patient-Reported Outcome and Supportive Care
Optimizing Skeletal Health: A Retrospective Analysis of Bone-Modifying Agent Prescription Patterns and Incidence of Skeletal-Related Events in Multiple Myeloma
(PA-123) Optimizing Skeletal Health: A Retrospective Analysis of Bone-modifying Agent Prescription Patterns and Incidence of Skeletal-related Events in Multiple Myeloma

Nicole M. Sequeira, MBBS (she/her/hers)
Resident Physician, Internal Medicine
UConn Health
Introduction:
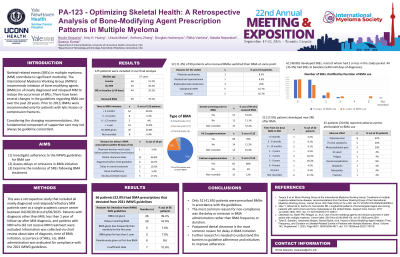
Skeletal-related events (SREs) in multiple myeloma (MM) contribute to significant morbidity. Bone-modifying agents (BMAs) are a fundamental component of bone disease treatment in MM. The impact of BMA prescribing patterns on SREs remains an area of ongoing investigation. The primary aims of this study are to investigate adherence to the International Myeloma Working Group (IMWG) guidelines for BMA use, assess delays or omissions in BMA initiation and examine the incidence of SREs following BMA treatment.
Methods:
We conducted a retrospective study that included all newly-diagnosed and relapsed/refractory MM patients seen at a single academic cancer center between 04/28/2018 to 01/06/2025. Patients with diagnosis other than MM, less than 1 year of follow-up after diagnosis, and no MM treatment were excluded. Time from diagnosis to BMA initiation and reason for delay were evaluated, as well as rationale for switching between different BMAs. BMA administration was evaluated for compliance with the 2021 IMWG guideline. Total numbers of SREs were calculated and stratified by duration of BMA use, and new SREs after BMA use were assessed.
Results: 127 patients were included in our final analysis. Median age was 67 years and 50.8% were female. 58 (45.6%) developed SREs during the study period, and the majority of these patients (45 patient, 36.2%) only had one SRE event. 44 patients (32.8%) had SRE at baseline (within 60 days of diagnosis). 99 patients (77.9%) were prescribed BMA after diagnosis of MM (73.4% zolendronate and 18.2% denosumab). Among these, 53 patients (53.6%) received BMA within 3 months. 38 (29.9%) had delays in BMA initiation, most commonly due to delayed dental clearance (14, 34.1%), physician decision (5, 12.2%), and patient refusal in (5, 12.2%). A total of 12 patients switched BMA type, with suboptimal eGFR (5 patients, 41.7%) being the top reason. 51 patients (48.1%) received dental screening before BMA initiation. 22 (16.4%) patients developed SREs after BMA treatment, with most events (8 cases, 36%) between 2 and 5 years after the first dose of BMA. 24 (17.9%) patients suffered relapse, among which 18 (75%) received BMA. Number of SREs followed a similar distribution for BMA duration ≥ 5 years versus < 5 years. Overall, 67 (52.7%) patients had BMA prescriptions that deviated from the IMWG guideline, most commonly due to delayed (25 patients, 45.4%) or omitted (22 patients, 40%) administration.
Conclusions:
Less than 50% of BMA prescribing practices were consistent with the guideline. The most common reason for non-compliance was delay or omission in BMA administration rather than BMA frequency or duration. Postponed dental clearance is the most common reason for delay in BMA initiation. More than one-third of patients developed SREs following BMA treatment, particularly between two to five years after the first dose, which is comparable to previous studies. Future studies may look into initiatives to improve guideline adherence.
